Night Operation
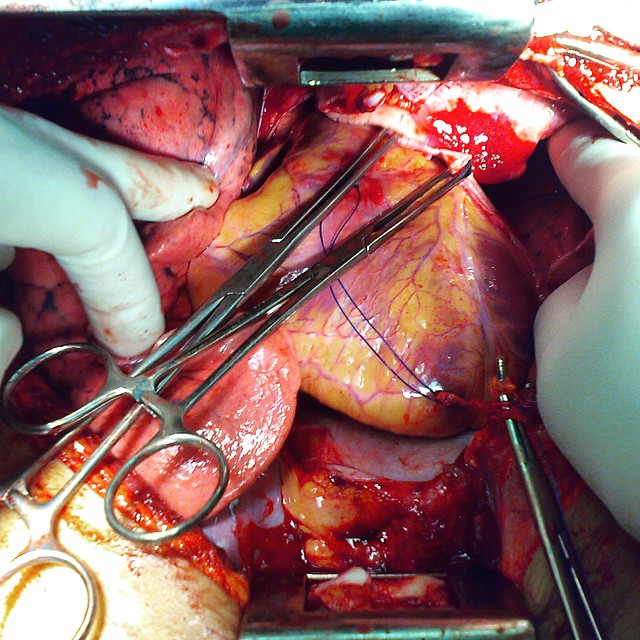
A typical picture of GIST (Gastrointestinal Stromal Tumor) from a patient that went through a subtotal gastrectomy.
GISTs are pretty common mesenchymal neoplasms of the GI tract. They are tumors of the connective tissue, which means that they are non-epithelial in origin, and are associated with several genetic mutations such as c-KIT mutations in more than 80% of the cases. The patient might have GI bleeding, trouble swallowing, intestinal obstruction and metastases to the adjacent organs (mainly to the liver). Surgical resection is the primary treatment of choice when a resectable GIST is present, although medications can be useful as well.
Surgical excision of a liver tumor. Hepatoblastoma is a rare cancerous tumor of the the liver that mainly affects children and does not spread outside of the liver, but rare cases of metastasis do occur, with the lung being the predominant site of metastases both at presentation and relapse. The etiology is unknown, although some genetic conditions has been associated with an increased risk for developing hepatoblastoma, including Beckwith-Weidemann syndrome, familial adenomatosis polypi, Wilson disease and other conditions like low birth weight and inborn errors of metabolism as are the glycogen storage diseases. Symptoms can vary depending on the size and location of the tumor and whether or not metastasis occurred. These are swollen abdomen, fever, weight loss, nausea, vomiting, abdominal pain and jaundice. The primary treatment is surgical resection, however, chemotherapy plays an important role by increasing the number of tumors that are resectable. The prognosis for patients with resectable tumors is fairly good, however, the outcome for those with nonresectable or recurrent disease is poor.
Intraoperative urgent control for a biventricular shotgun injury of the heart with the involvement of major coronary arteries, the proximal RCA and LAD (Right Coronary Artery and Left Anterior Descending, respectively).
!!!Viewer discretion is advised!!! Who's in for a new face?
A face transplant, partial or full, is a pretty promising branch of the modern medicine. People with faces disfigured from a traumatic injury, burns, disease, or even birth defects benefit from the procedure. Surgeons must consider both form (how the skin, bones and underlying musculature looks) and function of remaining tissue (if major components like jaw, lips, nose and eyelids are still intact). Don't mix face transplant with a face reconstruction, which is basically moving the patient's own skin (an autograft) from their back, buttocks, thighs, or chest to their face in a series of many procedures in order to regain even a small fraction of functionality.
Furthermore, face donation is not included in the commonly used driver's license organ donation registry. It requires a special and sensitive consent process with the donor families.
Skin grafts are often employed after serious injuries when some of the body's skin is damaged. Surgical removal (excision or debridement) of the damaged skin is followed by skin grafting.
The grafting serves two purposes: reduce the course of treatment needed (and time in the hospital), and improve the function and appearance of the area of the body that receives the skin graft. There are two types of skin grafts, the more common type is the split-thickness graft where a thin layer, the epidermis, is removed from a healthy part of the body (the donor section) like peeling a potato, or a full thickness skin graft, which involves the removal of both epidermis and dermis away from the donor section. A full thickness skin graft is more risky, in terms of the body accepting the skin, yet it leaves only a scar line on the donor section. For full thickness skin grafts, the donor section will often heal much more quickly than the injury and is less painful than a partial thickness skin graft. In this case, a supra-clavicular full thickness skin graft was harvested to cover a part of the frontal area after the surgical resection of a squamous-cell carcinoma lesion.
Does this beauty over here look abnormal? What's your pathological diagnosis?
Update : Yeah, most of you got it right!
Hypertrophic cardiomyopathy is a condition in which the heart muscle becomes thick, especially of the ventricles (lower heart chambers), which is seen very clearly in this picture.
The average left ventricular wall thickness in normal adults is 1.1 cm, but there are exceptions. Trained athletes have hearts that have left ventricular mass up to 60% greater than untrained subjects, with an average left ventricular wall thickness of 1.3 cm.
The most common cause is hypertension. As many as 1/3 of patients show left ventricular hypertrophy of any degree along with hypertension.
Symptoms include dyspnea (shortness of breath) due to stiffening and decreased blood filling of the ventricles, exertional chest pain (angina) due to reduced or restricted blood flow to the coronary arteries, uncomfortable awareness of a fluttering or pounding heart beat (palpitations) due to the ischemia to the heart muscle, disruption of the electrical system running through the abnormal heart muscle, lightheadedness, fatigue, fainting (called syncope) and sudden cardiac death.
Treatment depends on the cause. Athletic hypertrophy does not require any treatment, they're simply advised to stop exercising for a few months to measure their left ventricle again. Hypertensive LVH is treated by controlling the blood pressure with medications and lifestyle changes.
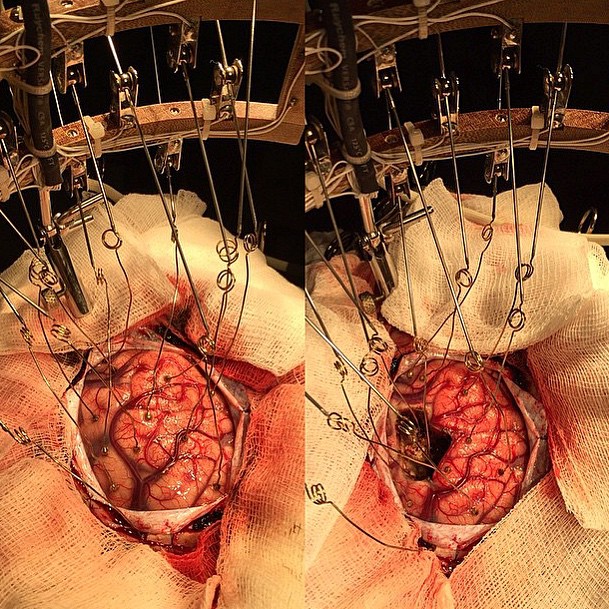
Intraoperative electrocorticography (ECoG) is a pretty valuable tool in epilepsy surgery, it is traditionally used in the surgical management of medically refractory partial epilepsies to identify the location and limits of the epileptogenic area and to guide the extent of resection for best seizure control.
The above photo shows an Intraoperative electrocorticography before and after resection of the epileptogenic zone.
Right hemicolectomy shaped like a heart! Nothing wrong with the surgeon being creative.
A right hemicolectomy, as shown here, involves removing the right side of the colon and attaching the small intestine to the remaining portion of the colon.
It's basically performed for patients with a colon cancer, or for certain non-cancerous conditions such as Crohn’s disease. In most cases the operation can be performed via a laparoscopic (keyhole) surgical technique.
How about some gyri and sulci? This is a photo of a fresh brain after it has been in formaldehyde solution for the purpose of hardening of the brain tissue, which is otherwise soft, and preservation of the brain cells.
As you know, cellular water is the major constituent of our bodies and its content varies in brain regions. This water plays a key role in cell regulation, its distribution is an accurate indicator of cellular structure as it interacts with different tissue components such as membranes and nerve fibers. The basic mechanism of formaldehyde preservation is that water movement is significantly reduced in the samples preserved with formaldehyde. This effect is due to cross-links between proteins which trap free water and reduce its mobility, makes it stiffer than it is.
Well, some people are keeping their body parts with them no matter what! "A guy just came in and I saw he was missing his little finger. So to make conversation I asked how he lost it... He replied I haven't lost it, it's in my pocket. He was telling the truth." A finger story by @marcwscwsdawson93
Are you ready for dissection?
Ok last one for this case! This is a postoperative picture after the successful resection of the meningioma.
The patient has completely recovered from her right lower limb weakness.












Yorumlar
Yorum Gönder